Summary of Insta-Live on @lyzevansphysio held Sunday 25/07/2021
Prepared by Dr Lynn Townsend, MBBS BSc(Hons) FRANZCOG DDU
Background:
COVID-19 is a serious illness and can lead to death or long term illness.
The risks of the illness to pregnant women include the respiratory complications (like the
general population) and pregnancy specific risks including miscarriage, abruption, abnormal
clotting and pre-eclampsia, which are all increased compared to the usual pregnancy risks.
As of 23/07/2021, RANZCOG and ATAGI recognised those increased risks and changed the
eligibility of pregnant women to 1b.
They have recommended mRNA vaccination in pregnancy. The only currently available
mRNA vaccine at present is the Pfizer BioNTech vaccine, however from September the Moderna vaccine has been reported to be available in Australia.
Historical background of mRNA technology:
mRNA technologies have developed since 1990 and the methods of producing mRNA technologies has improved dramatically since that time.
The technology has been used to develop vaccinations for infectious agents, cancer- vaccinations and immunomodulator therapies.
Many vaccinations have been developed using this technology but as yet have not been released to the public as there are already cheap effective alternatives, and scientific funding has always been difficult to obtain.
COVID-19 presented the world with a great challenge and the funding and scientific interest in this disease has meant that many laboratories were able to work on a COVID-specific vaccination, using the tools that they were already developing.
How do mRNA vaccines work?
All vaccinations rely on the premise that our natural immune system, mediated by B and T cells, recall “non-self” proteins and produce antibodies and cells to remove those proteins and neutralise them.
Older vaccines relied on using whole, inactivated cells or viral particles to expose to the immune system and then allow the immune system to remember how to neutralise that threat.
More contemporary vaccines rely on introducing protein fragments to the immune system and allowing the system to activate the neutralising and remembering “protocols”.
mRNA vaccines work by introducing tiny pieces of genetic code into the body. The cells that neutralise the code fragments are co-opted into producing the protein fragment which is then presented to the immune system and a response of neutralising and remembering is initiated.
The mRNA fragments are then completely destroyed and are no longer detectable after 48- 72 hours.
These fragments are unable to be incorporated into any genetic material within the body’s cells. The protein they produce are recognised as “non-self” and completely neutralised and remembered.
When a person is then exposed to “wild” COVID-19, the immune system swings into action and produces antibodies which neutralise the wild virus.
The COVID-19 vaccines, whilst helping to reduce the likelihood of disease have definitely reduced the likelihood of hospital or ICU admission.
Risk-Benefit matrix of Obstetric patients:
The initial mRNA vaccinations for COVID-19 were clearly demonstrated, using established Phase 1- 3 testing, to be safe and effective for non-pregnant people.
In some populations, the risk of COVID-19 at the end of 2020 and beginning of 2021 was very high, and pregnant women consented to getting vaccinated, understanding that the biological likelihood of adverse events was low and the potential benefit of the vaccine were high.
This occurred largely in the USA and Israel, but other countries such as Scotland also vaccinated their pregnant population.
After 6 months of active vaccination programs, we now have a population based database of large numbers of pregnant women having the vaccine.
o In the USA as of late July 2021, approximately 150000 pregnant women have been vaccinated, primarily with mRNA vaccines.
o We are uncertain how many actual pregnant women have been vaccinated worldwide, and we are uncertain which vaccine they received.
o It is highly likely that many more have been vaccinated in countries like China and Russia, using their locally developed vaccinations.
• In the literature, various analyses of outcomes have been published.
o The largest group was based in the USA and examined nearly 36000 women.
They found no increase in pregnancy and neonatal outcomes compared to the usual expected background rate of these conditions. This was published in a very high quality peer reviewed journal (NEJM) in June 2021.
o In Israel, nearly 7500 women were immunised and again, they found no increase in pregnancy complications and a significantly lower risk of infection in the vaccinated group. This was published also in a very high quality peer reviewed journal (JAMA) in July 2021.
o Lastly, in Scotland, almost 4000 pregnant women were immunised and they found similar outcomes. Their findings are still in press.
Pregnancy Specific Concerns:
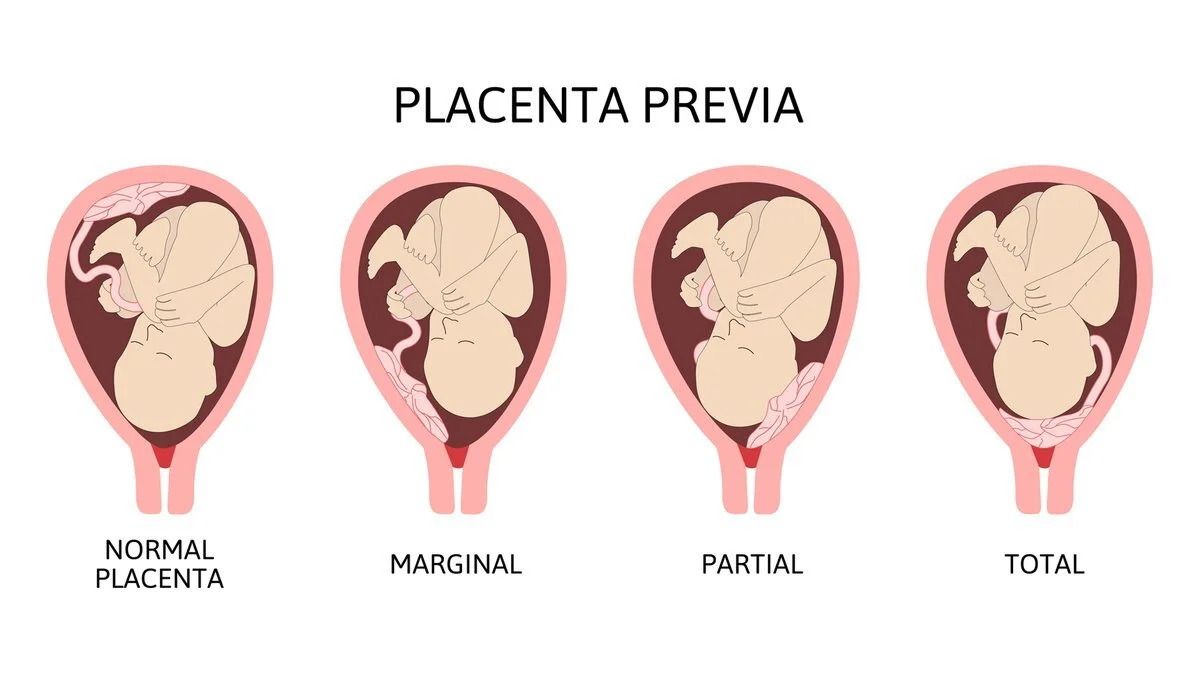
No difference in all pregnancy outcomes
Good quality histological evidence of NO placental effects of the vaccine.
No mRNA crosses the placenta, only the maternally generated antibodies
There are detectable levels of maternal generated antibodies in cord blood which help to
protect the baby in the first few weeks of life.
Breastfeeding:
Maternally derived antibodies cross into the breastmilk and also protect the baby via passive
immunisation.
No mRNA fragments are detectable in the breastmilk.
No need for “pump and dump”
Fertility:
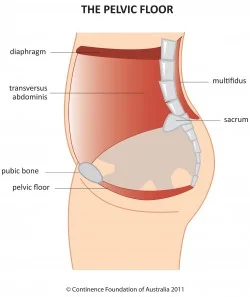
No interaction of the mRNA fragments with the female or male genitourinary system
No evidence of impact on fertility (IVF) treatments
Consequently, the current recommendation is that women should be vaccinated if eligible,
during fertility treatments and should not delay becoming pregnant.
Other key points:
All data is based on mRNA vaccines, so pregnant women should only consider Pfizer at present in Australia, not AZ
AZ still is an excellent, safe vaccine in appropriate groups after medical assessment.
“Long covid” is a post-viral illness that causes significant consequences with extreme fatigue
and other prolonged symptoms that can significantly impact normal life activities. There is some evidence that even people with long covid benefit from vaccination as it can reduce the effects.
References:
How do mRNA vaccines work?
Pardi, N., Hogan, M.J., Porter, F.W. and Weissman, D., 2018. mRNA vaccines—a new era in
vaccinology. Nature reviews Drug discovery, 17(4), pp.261-279. USA Cohort study assessing pregnancy risk of vaccination
vaccine safety in pregnant persons. New England Journal of Medicine, 384(24), pp.2273-2282. Israeli Cohort study assessing pregnant risk of vaccination
Shimabukuro, T.T., Kim, S.Y., Myers, T.R., Moro, P.L., Oduyebo, T., Panagiotakopoulos, L., Marquez,
P.L., Olson, C.K., Liu, R., Chang, K.T. and Ellington, S.R., 2021. Preliminary findings of mRNA Covid-19
Goldshtein, I., Nevo, D., Steinberg, D.M., Rotem, R.S., Gorfine, M., Chodick, G. and Segal, Y., 2021.
Association Between BNT162b2 Vaccination and Incidence of SARS-CoV-2 Infection in Pregnant
Women. JAMA. And also:
Burd, I., Kino, T. and Segars, J., 2021. The Israeli study of Pfizer BNT162b2 vaccine in pregnancy:
considering maternal and neonatal benefits. The Journal of Clinical Investigation.
And also:
Bookstein Peretz, S., Regev, N., Novick, L., Nachshol, M., Goffer, E., Ben-David, A., Asraf, K.,
Doolman, R., Sapir, E., Regev Yochay, G. and Yinon, Y., 2021. Short-term outcome of pregnant
women vaccinated by BNT162b2 mRNA COVID-19 vaccine. Ultr
Vaccination and placentation
Shanes, E.D., Otero, S., Mithal, L.B., Mupanomunda, C.A., Miller, E.S. and Goldstein, J.A., 2021.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination in pregnancy: measures
of immunity and placental histopathology. Obstetrics & Gynecology, pp.10-1097. Vaccination and ferility:
Safrai, M., Rottenstreich, A., Herzberg, S., Imbar, T., Reubinoff, B. and Ben-Meir, A., 2021. Stopping
the misinformation: BNT162b2 COVID-19 vaccine has no negative effect on women’s
fertility. medRxiv. And also:
Mattar, C.N., Koh, W., Seow, Y., Hoon, S., Venkatesh, A., Dashraath, P., Lim, L.M., Judith, O.N.G., Lee,
R.J., Johana, N. and Yeo, J.S., 2021. Addressing anti-syncytin antibody levels, and fertility and
breastfeeding concerns, following BNT162B2 COVID-19 mR
asound in Obstetrics & Gynecology.
NA vaccination. medRxiv.
Australian Government Decision Guide (an excellent reference)
https://www.health.gov.au/sites/default/files/documents/2021/06/covid-19-vaccination-shared- decision-making-guide-for-women-who-are-pregnant-breastfeeding-or-planning-pregnancy-covid- 19-vaccination-shared-decision-making-guide-for-women-who-are-pregnant-breastfeeding-or- planning-pregna_0.pdf