The placenta develops at the same time as your baby and is attached to the lining of your uterus (womb) during pregnancy. It allows for oxygen and nutrients to pass from you to your baby as well as producing hormones that support your pregnancy.
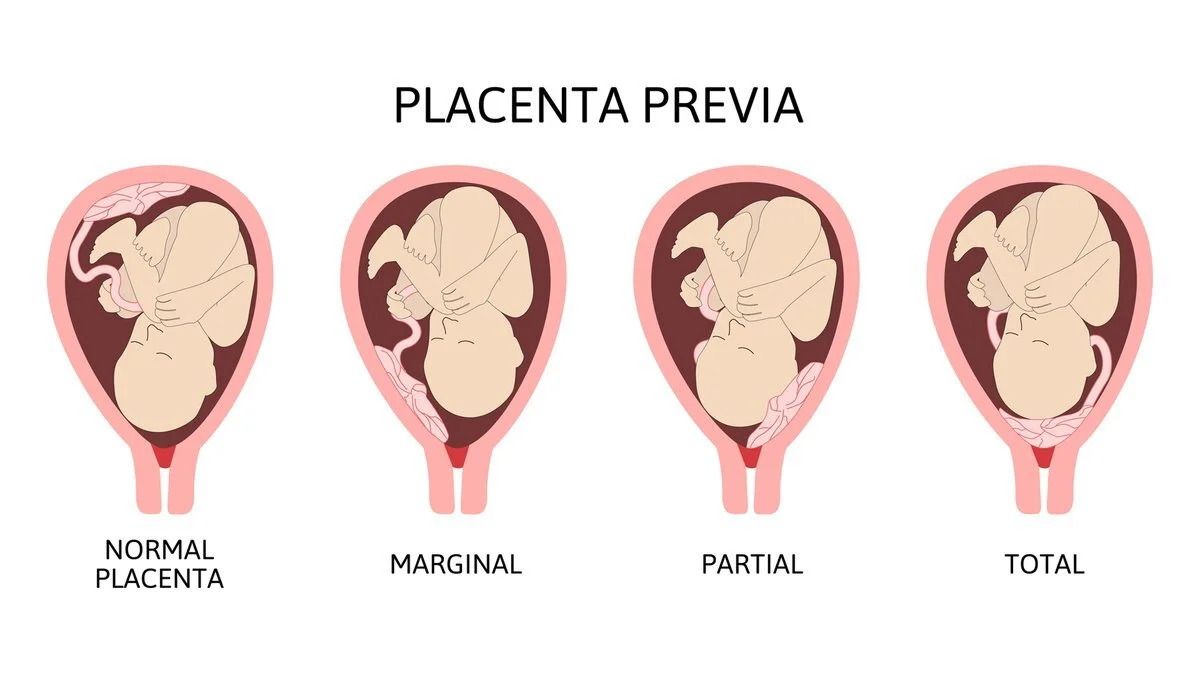
Placenta praevia means the placenta has implanted at the bottom of the uterus, covering the cervix.
When a baby is ready to be born, the cervix (neck of the womb) dilates (opens) to allow the baby to move out of the uterus and into the vagina. When a woman has placenta praevia (the placenta has implanted at the bottom of the uterus, over the cervix or close by), the baby can’t be born vaginally. ‘Partial placenta praevia’ means the cervix is partly blocked, while ‘complete placenta praevia’ means the entire cervix is obstructed.
Some of the causes include scarring of the uterine lining (endometrium) and abnormalities of the placenta. Around one in every 200 pregnancies is affected.
Symptoms of Placenta Praevia
The most important symptom in placenta praevia is painless vaginal bleeding after 20 weeks. However, there are causes of vaginal bleeding other than placenta praevia. All bleeding during pregnancy should be reported to your doctor for prompt investigation and treatment.
Placenta Praevia Treatment
Placenta praevia is graded into 4 categories from minor to major. If you have grade 1 or 2 it may still be possible to have a vaginal birth, but grade 3 or 4 will require a caesarean section.
Any grade of placenta praevia will require you to live near or have easy access to the hospital in case you start bleeding. Heavy bleeding may mean you need to be admitted to hospital for the remainder of your pregnancy.
When you are in hospital, your blood will be taken to make sure an exact donor blood match is available in case you need a blood transfusion. You may also need to take iron tablets if you have anaemia (low blood haemoglobin level).
If you have bleeding during your pregnancy and have Rh negative blood, you will need an injection of Anti D so your baby is not affected by the bleeding.
Your baby may also be monitored with a cardiotocograph (CTG) to make sure they are not distressed. The CTG records your baby's heart rate and response to movements and contractions.
Being in hospital doesn't stop you from bleeding, but your baby can be delivered more quickly if needed. Your doctor or midwife will discuss any test results with you and what steps may be needed to ensure you and your baby's wellbeing.
Things to remember
During pregnancy, the placenta provides the growing baby with oxygen and nutrients from the mother’s bloodstream.
Placenta praevia means the placenta has implanted at the bottom of the uterus, over the cervix or close by, which means the baby can’t be born vaginally.
Treatment aims to ease the symptoms and prolong the pregnancy until at least 36 weeks.